There are many possible causes of liver disease. Some can be sudden and severe, while others progress slowly over time. Any cat can be affected and this condition is serious.
When the liver is not working properly, damaging byproducts of metabolism can build up in the body. At the same time, important body functions may start to fail. Other organs can be affected, particularly the brain. Because of all this, there are many possible types and symptoms of liver disease. The liver is very good at healing after being damaged, but it can sometimes be overwhelmed and failure can progress rapidly.
Overview
What is Liver disease?
The liver has many crucial functions, notably helping in digestion, eliminating toxins and producing many important proteins. The liver has huge capacity to deal with damage and heals quickly, so minor damage may cause no symptoms or have a quick and full recovery. But when damage is severe or prolonged, many symptoms can develop. There are many types of liver disease in cats:
Acute liver failure
This happens when there is a sudden loss of liver function. It can be a complication of long-term disease, or be due to sudden damage to the liver by:
- Poisons: blue-green algae or aflatoxins from mould)
- Infections
- Side effects of drugs: some antifungals, anticonvulsants or anti-inflammatories)
This type of liver disease is very serious and requires immediate intensive care treatment.
Hepatic lipidosis
- Can develop when cats do not eat for several days, especially if they are also otherwise unwell.
- When fat stores from around the body are mobilised to the liver to be turned into usable energy, the liver becomes overwhelmed and fat starts to build up within it, replacing normal liver cells.
- This gets in the way of other liver functions and damages the liver further.
- Detecting this complication early and providing nutritional support, usually with a feeding tube, is an essential part of treatment.
Neutrophilic cholangitis and cholecystitis
- Sometimes referred to as Feline Cholangitis/Cholangiohepatitis Syndrome or triaditis.
- It is thought that bacteria travel from the small intestine, up the bile duct and into the gallbladder and liver.
- Severe inflammatory response develops in the gallbladder and progresses into the liver.
- Affects liver function as well as general health.
- Most cases develop suddenly, but some can go on to become chronic disease.
Lymphocytic cholangitis
- Long-term inflammation of the liver.
- Thought to be caused by the immune system, although it is possible bacteria may initially set off the problem.
- Diagnosis usually requires a biopsy.
- Treatment is with immunosuppressive drugs such as steroids, alongside supportive care.
Abnormal blood flow through the liver (Portosystemic shunts)
- Hereditary condition: Some cats may be born with abnormal blood vessels that go around instead of through the liver.
- Can also develop as a complication of other types of liver disease.
- Allows anything absorbed through the gut to reach other organs, like the brain, without being processed by the liver first.
- Can cause episodes of severe disease and may need to be corrected with surgery.
- Not a common problem in cats.
Infections affecting the liver
- Infections specifically affecting the liver are rare in cats, many infections that affect multiple organs can affect the liver.
- Examples are Infectious Feline Peritonitis and Toxoplasmosis.
- The primary treatment is directed to the infection, but liver support may also be necessary.
Liver cancer
- Primary liver tumours are uncommon in cats, but more common than spread from other organs.
- Of these, benign tumours are more common, especially in older cats.
- Symptoms will depend on the specific type of tumour.
- Lymphoma can sometimes be localised to the liver in cats or affect multiple organs. This can be serious but chemotherapy can sometimes be effective.
Diseases of the gallbladder
- Bile is very important for digestion. It is produced in the liver and stored in the gallbladder.
- Small tubes lead the bile from the liver to the gallbladder, and then a bigger one that takes the bile from there to the small intestine (the bile duct). The pancreas is in this area as well.
- This proximity and communication makes it common for the pancreas, small intestine, gallbladder and liver to affect each other, and many cats suffer from cholangitis, cholecystitis, pancreatitis and inflammatory bowel disease at the same time.
- Obstruction of the bile duct is a rare but severe condition that can cause sudden liver failure.
Symptoms
Symptoms of liver disease
Symptoms of liver disease depend on the underlying cause. Many symptoms are common across different conditions.
Sudden liver disease may cause:
- Vomiting and diarrhoea
- Lethargy
- Not wanting to eat
- Excessive drooling
- Jaundice (yellow tinge to the gums, skin and white part of the eyes)
- Bruising
- Weakness
- Abnormal behaviours
- Seizures
Long term liver disease may cause:
- Weight loss
- Reduced appetite
- Changes to thirst and volume of urine produced
- Vomiting and diarrhoea
- Lack of energy
- Behaviour changes
- Blood in vomit or stool
- Bruising easily
Risk
Cats at higher risk of liver disease
- Liver disease can affect any cat.
- Cats with a weakened immune system are at higher risk of developing secondary infections that affect the liver and gallbladder.
- The issues with the immune system may be present at birth or be due to Feline immunodeficiency virus, Feline leukaemia virus or some medications.
Diagnosis
Diagnosis of liver disease in cats
Recognising recent liver damage is usually quite straightforward. After a detailed history and physical exam, your vet will request:
- Blood tests: to measure the levels of several parameters that relate to liver disease.
- ALT (alanine transaminase)
- AST (aspartate transferase)
- ALKP (alkaline phosphatase)
- GGT (gamma-glutamyl transferase)
- Bilirubin: produced when red blood cells degrade, is normally excreted by the liver. It can also deposit on the skin, gums, and the white of the eyes, and it causes jaundice.
- Bile acids: measured before and after a meal, are one of the best tests to assess liver function.
- Protein, BUN and Cholesterol levels: if low can be a sign of poor liver function in long-term disease.
- Ammonia levels: measured when brain symptoms are present, such as seizures or abnormal behaviours, to assess if the liver is the cause.
- Coagulation tests: performed if blood clotting issues are noted or if liver disease is suspected and surgery is needed..
- Ultrasound scan, CT scan or MRI: to check for masses and general appearance of the liver and gallbladder. These tests cannot diagnose a specific cause or or determine how severe the problem is. They allow the diagnosis of blood vessel abnormalities or gallbladder stones.
- Sampling the liver: Taking a small sample of the liver is usually the only way to know the cause of a long-term liver problem. This is often necessary to be able to choose the right treatment. This can be done by:
- Fine needle aspiration through the skin. This only obtains a very small sample but can be enough to diagnose some conditions, such as hepatic lipidosis.
- Biopsy through the skin. This obtains a slightly bigger sample and provides much more information, but it is very easy to miss major changes and have the wrong diagnosis.
- Biopsy during endoscopy or surgery. This provides the most accurate information but is a more complex procedure.
Vet treatment
Vet treatment of liver disease
Treatment of liver disease will depend on the cause of the problem. Some medications benefit most patients with liver disease:
- Acute liver problems
- Antibiotics, if cholangitis or cholecystitis is suspected or has been confirmed
- Removal of any toxin or drug causing liver damage (see intoxication in cats)
- Fluids via a drip to correct dehydration and electrolyte imbalances
- Anti-vomiting medication
- Pain medication when necessary
- Chronic liver problems::
- Special diet to reduce the workload of the liver and provide nutrients to help it heal
- Medications or supplements that support liver function, such as:
- Ursodeoxycholic acid: promotes the flow of bile and may protect liver cells from damage
- S-Adenosyl methionine (SAMe): a supplement that is thought to help in the detoxifying functions of the liver and may help prevent further liver damage
- Silymarin: a supplement derived from milk thistle. It has antioxidant properties and is also thought to help prevent liver damage.
- Vitamin K: if clotting is being affected or a deficiency is detected
- Steroids: for cases of lymphocytic cholangitis
- Surgery may be needed for:
- Portosystemic shunts
- Removal of masses
- Obstruction of the gallbladder
- Chemotherapy: if a tumour in the liver has been diagnosed
Home treatment
Home treatment of liver disease in cats
- Because of the multiple functions of the liver and complexity of many liver conditions, treatment often involves balancing different aspects and interventions.
- Dietary changes and supplements are a fundamental part of the treatment of long-term disease, especially liver disease.
- Discuss diet and supplements with your vet to find the right option for your cat and make sure all aspects of the treatment plan are considered together.
- Even natural treatments may interact with liver functions or other treatments and cause unexpected things to happen. Discuss these thoroughly with your vet to avoid complications.
Prevention
Can liver disease be prevented? Can my family catch it?
- Liver disease has many possible causes and most of them cannot be directly prevented.
- A healthy and balanced diet promotes liver health and also general health.
- Cats on long-term medication that may affect the liver, such as steroids or certain epilepsy treatments (phenobarbital) , should have regular blood tests to monitor liver function and catch any potential problems early.
- The types of liver diseases that usually affect cats are not contagious to other animals or people.
When to worry
When to worry about liver disease in cats
Take your cat to see a vet immediately if they develop:
- Seizures
- Yellow gums, skin or eyes
- Large amounts of blood in their vomit or diarrhoea
- Black or tarry stools
- Constant vomiting
- Weakness or lack of response when you interact with them
Speak to a vet as soon as possible if your cat:
- Develops abnormal behaviours
- Is drinking excessive amounts of water or urinating constantly
- Loses interest in food and has not eaten for more than a day
- Develops unexplained bruises
- Is quiet or lethargic
- Has vomiting or diarrhoea, especially if containing blood.
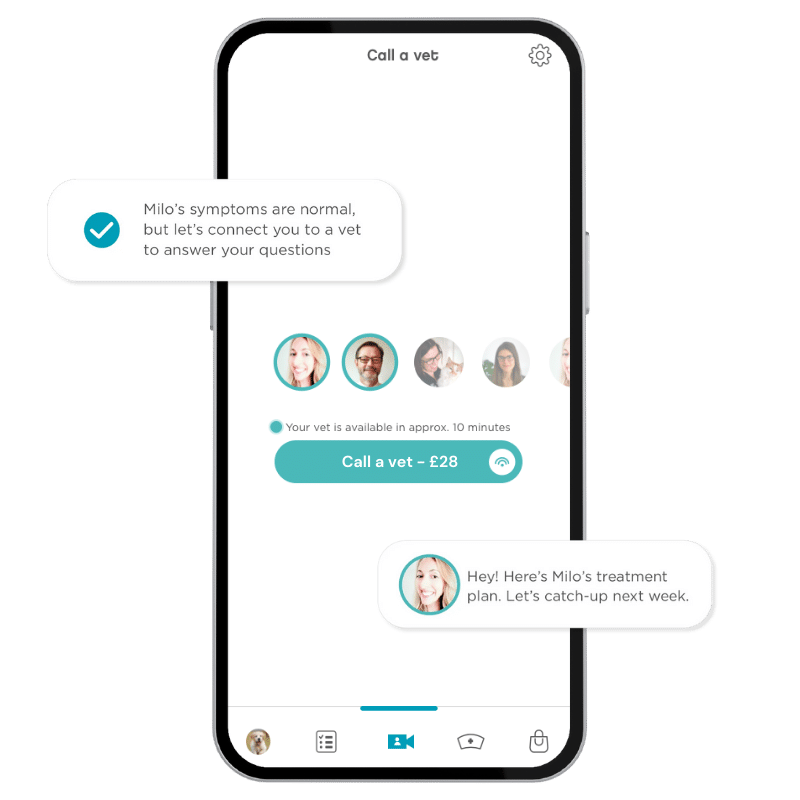
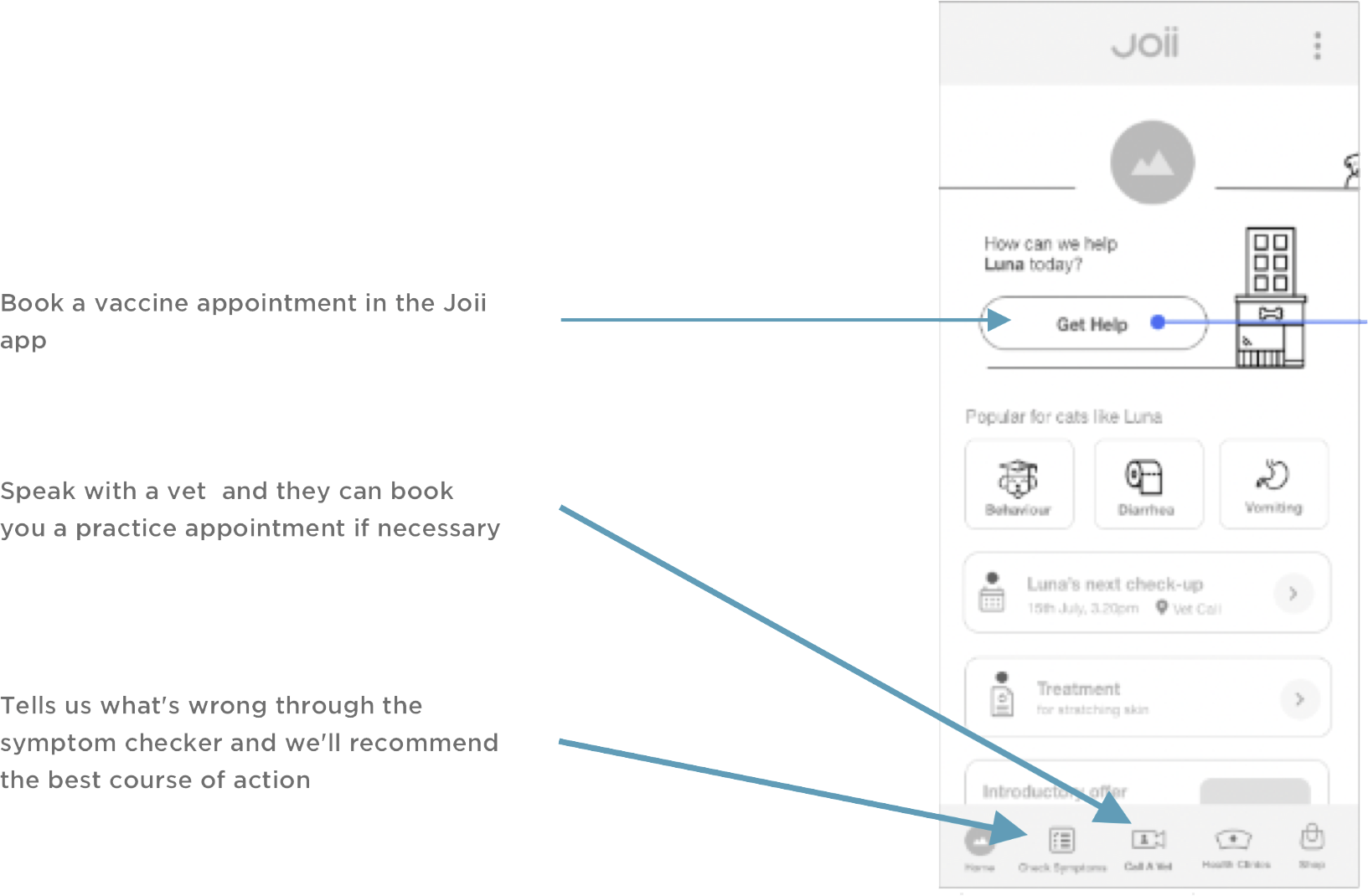
The vets and nurses at the Joii app are always available to give you advice and answer any doubts.